40 yr Old female with CHOLELITHIASIS.
THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT.
THIS E BLOG ALSO REFLECTS MY PATIENT CENTERED ONLINE LEARNING PORTFOLIO AND YOUR VALUABLE INPUTS ON THE COMMENT BOX IS WELCOME.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 40year old female patient presented to the OPD complaining severe pain in the abdomen region since morning (25/02/2022)
CHEIF COMPLAINTS:-
Patient was apparently asymptomatic se
C/o pain abdomen since 2 years.
She is a housewife and she was detected 4 years earlier. But the pain started getting worse since 2 years. She has been medicated under local doctor provision.
HISTORY OF PRESENT ILLNESS :-
Patient came with bloating and then developed abdomen pain.
HISTORY OF PAST ILLNESS:-
Not a k/c/o DM, HTN, TB, BA, CAD, CVA.
PERSONAL HISTORY:-
Appetite- Normal
Diet- Mixed
Bowels and bladder -Regular
Micturition- Normal
Allergies-No
No habits.
FAMILY HISTORY:-
Allergic history :- not known case of allergy
Not allergic to pollen, and any known drugs.
TREATMENT HISTORY:- Non Significant
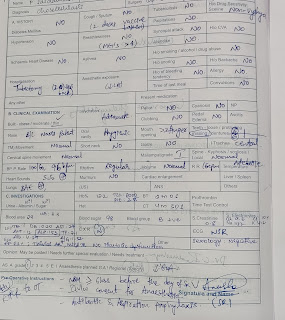
GENERAL EXAMINATION:-
Patient is conscious,coherent,cooperative.
Vitals at admission:-
Temperature:- Afebrile
Pulse rate :-80/min.
Respiration rate:-12/min.
BP:- 110/80 mmHg.
SpO2:- 98%
SYSTEMIC EXAMINATION:-
Cardiovascular systems:- S1 S2 heard, No murmurs.
P/A soft :- Tenderness in right hypochondria.
Respiratory system:- No rigidity
Breath sounds -vesicular.
Abdomen:-
Tenderness,
Bowel sounds-Yes
PLAN OF CARE:-
Laproscopic cholecystectomy
DRUGS REQUIRED FOR GENERAL ANESTHESIA:-
Preanesthetic assessment:-
INVESTIGATIONS:-
ECG REPORT:-
COMPLETE URINE EXAMINATION :-
COMPLETE BLOOD PICTURE:-
BLOOD GROUPING AND Rh TYPE:-
BLOOD- SUGAR RANDOM:-











Comments
Post a Comment